Bipolar disorder, or manic depression, is a mood disorder.
A person with bipolar disorder experiences phases of extreme mood swings
between debilitating lows of depression and euphoric highs called mania.
Understanding bipolar disorder can make a dramatic difference on how this
mental illness is viewed. The majority of information found about bipolar
disorder may seem negative, but there are many positive attributes that can
manifest from having this disorder. There is no cure for bipolar disorder. Palliative
care focuses on treating the symptoms of the disorder so the individual becomes
functional in life. Bipolar disorder is a complicated disease that
can be managed with knowledge, understanding, and patience. This
research paper will emphasize the following categories: statistics,
diagnostic criteria, non-adherence to treatment, coping skills, and positive
attributes of the disorder.
Two sources contain statistical information. “Bipolar
Disorder Statistics” from the website StatisticBrain.com gives statistical
information on bipolar disorder as verified by the DBS (Depression and
Bipolar Support) Alliance, Bipolar ism [sic], and Bipolar Lifestyles. It
states 5.7 million adults, or 5% of the population suffers from bipolar
disorder. When one parent has the condition there is a 23% chance that it
will be passed down to their child. The probability that a child will
inherit the condition increases to 66% if both parents posses the
illness. The occurrence of suicide related to the disease is 20%, reducing
the average life-span by 9.2 years. 70% of people with bipolar disorder
will receive at least one misdiagnosis. The other source with the same
title, “Bipolar Disorder Statistics” by DBS Alliance shows statistics for
bipolar depression as reported by NIMH (National Institute of Mental Health)
and the World Health Organization. Although the median age of the onset
of bipolar disorder is 25, the illness can begin in early childhood or as late
as 40 to 50 years old. More than two-thirds of people with bipolar
disorder have at least one close relative who possess the illness which suggests
the disease has a heritable component. Bipolar disorder is the sixth
leading cause of disability. Adolescents with major depression develop
the disorder within five years of the onset of depression 20% of the
time. It is suggested that up to one-third of the 3.4 million children
and adolescents in the United States with depression may be experiencing the
early stages of bipolar disorder.
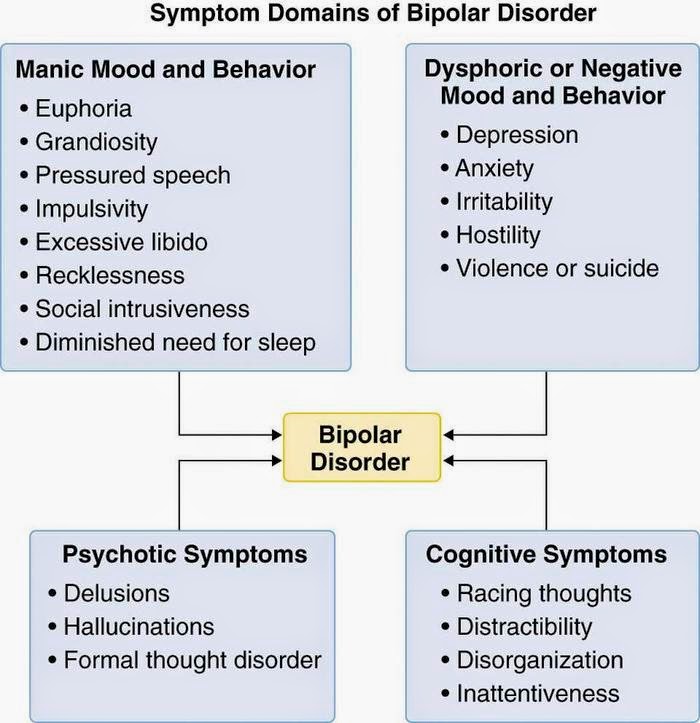
Using diagnostic criteria,
it is difficult to accurately diagnose bipolar disorder. In order to
describe bipolar disorder, it is necessary to first discuss the symptoms of
depression. According to the booklet “Understanding Bipolar
Disorder and Recovery” written by Ken Duckworth and distributed by NAMI
(National Alliance of Mental Illness) clinical depression, or unipolar
depression, is more than just feeling a normal sense of sadness. Major
depression is a medical disorder that makes it difficult to function in life.
People who are depressed typically have feelings of hopelessness, helplessness,
and worthlessness. The symptoms of depression are:
Cure Talk, Jul. 2013.
It is important to get
an accurate diagnosis to rule out other possible conditions that mimic
depression, such as hypothyroidism, complications from substance abuse or
dependence, anemia, and certain neurological disorders. Other psychiatric
conditions may resemble manic depression such as dementia, post-traumatic stress
disorder, schizophrenia, and ADHD (attention deficit hyperactivity disorder).
A person must exhibit both depressive and manic symptoms for the
diagnosis of bipolar disorder to be made.
Cleveland Clinic Foundation, Aug. 2010.
In addition, “Understanding Bipolar Disorder and
Recovery” emphasized that mood disorders are classified into two separate
categories, unipolar and bipolar disorders. Individuals who experience
unipolar disorder exhibit depressive symptoms, but never experience the highs
of mania. Although they are both considered to be mood disorders, they are
different illnesses. A person with bipolar disorder experiences mood
swings between the lows of depression and the highs of mania with normal
periods of mood in between.
People without the mood disorder do not have the exaggerated mood swings associated with
bipolar disorder. The moods of these individuals remain stable in the
normal range. Some people feel that they do not suffer from clinical
depression because their symptoms are short lived. They believe that they
only experience SAD (seasonal affective disorder) or postpartum
depression. They do not realize that the period when they are not
experiencing the symptoms of depression are the actually the normal stage
between depression and mania or the cycles of hypomanic or hypermanic phase.
Duckworth also discussed the topic of
co-morbidity. In psychiatry, this term is used when an individual
exhibits two or more psychiatric disorders at the same time. People with
bipolar disorder are vulnerable to anxiety disorders, alcoholism, substance
abuse, bulimia, ADHD, and migraine headaches. Successful treatment can
display improvement of these conditions. However, drug therapy for the
other conditions can cause negative effects in people with bipolar
disorder. For example, antidepressants used to treat obsessive-compulsive
disorder or stimulants for ADHD can worsen symptoms of bipolar disorder,
possibly causing a manic episode. When this occurs, other avenues of
treatment can be utilized. Manic depression is an illness that can reduce
quality of life and often is associated with many challenges.
It is common knowledge that prescription drugs have
negative side effects. Many commercials and magazine advertisements for
these medications warn to consult a physician if a patient has a history of
depression, experiences a change of mood or behavior or thoughts of
suicide. These drugs have been known to cause people with undiagnosed
bipolar disorder to enter into a major manic phase.
A report published by the University of Maryland Medical Center
titled “Bipolar Disorder” examined the different categories of the disorder and
the risk factors associated with the illness. Bipolar disorder is
classified into many different categories according to the pattern and severity
of symptoms. There are two main types. Bipolar I is characterized
by at least one manic or mixed episode and one or more depressive episodes that
last at least seven days. Manic and depressive episodes follow a regular
pattern. These episodes are more acute and severe than the other
categories. Bipolar II is characterized by predominately major depressive
symptoms with occasional hypomanic episodes that last about four days.
Hypomanic symptoms of euphoria are less severe and do not last as long as
mania.
In addition, the journal article by Guy M. Goodwin and
colleagues, “ECNP Consensus Meeting. Bipolar depression. Nice,
March 2007” published in European Neuropsychopharmacology, suggested that bipolar
disorder usually manifests itself in the late teen years or early
twenties. It has been found that children and those is their early teens
who suffer from unipolar depression actually have bipolar depression. It
is not uncommon for children to be misdiagnosed with ADHD or ODD (oppositional defiant disorder). It has been expressed that early intervention can be beneficial to the
prognosis of the illness. The study illustrates that bipolar disorder is
a progressive illness that worsens over time.
Bipolar disorder is an illness that can reduce quality of life
and often is associated with many challenges. The research article by
Holly L. Peay and colleagues “Adaptation to Bipolar Disorder and Perceived Risk
to Children: A Survey of Parents with Bipolar Disorder” published in BMC (BioMed Central)
Psychiatry explored the perceptions of adults with the disorder and
examined the coping methods of parents who are at risk of passing on their
illness to their offspring. It expressed the heritability of bipolar
disorder and the emotional struggles that each parent may have in regards to
passing this debilitating disease to their children. Parents who had a
positive support system processed the ability to cope without experiencing self
blame and denial.
Susanne Gibson and colleagues analyzed the reasons why over half
of the participants in the study did not follow treatment recommendations in
“Understanding Treatment Non-adherence in Schizophrenia and Bipolar Disorder: A
Survey of What Service Users Do and Why” published in BMC Psychiatry.
This source documented the reasons why many people with bipolar disorder chose
not to follow medical advice. Patients may choose non-adherence or
unintentional non-adherence to treatment as prescribed because they felt that
they were “better”, did not like the side effects of medications, or felt that
they needed more energy to complete tasks and that skipping medication made
them feel more alert. Non-adherence leads to relapse of the illness that
can cause serious side effects, including suicide. Individuals were
willing to risk the negative aspects because they enjoy the perceived positive
experiences connected to the illness. Furthermore, patients viewed the
short-term results of not taking their medication as prescribed more important,
rather than the long-term effects of non-adherence.
In their research article “The Cost of Relapse for Patients with a
Manic/Mixed Episode of Bipolar Disorder in the EMBLEM Study” for Pharmacoecomonics,
Jihyung Hong and his colleagues did a study to analyze the substantial costs
and the economic impact of relapse of bipolar patients during a 21 month
maintenance phase. The costs involved include medications, psychiatric
consultation visits, out-patient treatment, and inpatient care. Indirect
costs may be incurred by lost productivity from family members caring for the
patient with the illness. The reoccurrence of the disorder may lead to
progressive functional deterioration, worsening treatment response, and clinical
prognosis. This demonstrated the importance for the patient to follow
medical advice to prevent relapse and worsening of the progression of the
disease. Doctors using the DSM-IV may misdiagnose
patients with unipolar depression, instead of bipolar depression, if the
patient is evaluated in a depressed state. This can lead to treatment
that has a poor outcome.
Despite the many effective treatments for bipolar disorder, many
patients find it difficult to adhere to treatment. However, “Insight in
Bipolar Disorder” written by Klára Látalová, M.D. Ph.D., for Psychiatric
Quarterly, illustrated the value of insight for bipolar disorder. The
association has shown better results in the treatment of the disorder.
Awareness about the disorder has led to patients adhering to treatment which
leads to better outcomes. Information is a factor in successful
treatment.
Acquiring necessary coping skills has a valuable impact in the lives of people with bipolar disorder and those who interact with them. In the book, Living with Someone Who's Living with Bipolar Disorder: A Practical Guide for Family, Friends, and Coworkers, authors Chelsea Lowe and Bruce M. Cohen, showed that having an understanding of the illness can help others not affected by the disease cope with the behavior of the person with bipolar disorder. Knowledge about the illness and possessing the skills on how to deal with the triggers that can worsen the behavior of the individual with bipolar disorder can make life easier for everyone involved. The importance of understanding, knowledge, and support is invaluable to coping with the everyday life of a person suffering with bipolar disorder. A basic understanding of the influence of communication is crucial. When communicating, it is important to show respect by listening to what they have to say. Be noncritical, positive, and provide praise. Avoid physical confrontation and give them space. Do not blame or belittle. Don't get involved with no-win arguments and know when to walk away (129). It is essential that everyone involved educate themselves on the symptoms, treatments, and the latest research.
In spite of the negative characteristics surrounding the
disorder, some patients consider some of the symptoms as positive. In her
book, Touched with Fire, Kay Redfield Jamison, Ph.D., cited many
works of people throughout history who suffer from bipolar disorder. She
described work from numerous famous people, both literal and visual
artists. According to journals and medical records at the time of their
lives, she showed the likelihood of the person having the disorder and how their
moods affected their personal and professional lives. She documented their
productivity and quality of work depending on the state of mood they were
experiencing during the creative process. Artistic temperament can be
closely associated with a characteristic of manic depression. “Another
argument set forth against an association between ‘madness’ and artistic
creativity is that a bit of madness and turmoil is part and parcel of the
artistic temperament, and the artists are just more sensitive to life and the
experiences of life than are other people.” (90) Some of the famous
people that were mentioned are poet Edgar Allan Poe, writer Charles Dickens, and
artists Vincent Van Gogh and Michelangelo.
Similarly, Tracy Pedersen's website article, "Benefits of Bipolar Disorder?" from psychcentral.com, described a study where some individuals experience positive effects with having bipolar disorder. Researchers investigated evidence and reported that some people value certain experiences associated with the disorder and would prefer to retain their condition. Some of the aspects of this illness can be considered highly valuable attributes in some people. The ability to achieve at high levels of success is extremely rewarding. One of the participants declared, "It's almost as if it opens up something in the brain that isn't otherwise there, and I see color much more vividly than I used to...So I think that my access to music and art are something for which I'm grateful to bipolar for enhancing. It's almost as if it's a magnifying glass that sits between that and myself." Some people believe that positive benefits could be acquired from the low points also, such as having increased empathy for the suffering of others. This article revealed some benefits of this illness and why some people refuse treatment.
For instance, in her article “Is There a Bright Side to Bipolar
Disorder?” from everydayhealth.com, Madeline Vann, MPH, described advantages of
bipolar disorder that are considered to be appealing to those who have the
condition. These characteristics include productivity, confidence, charm,
euphoria, and insight. Productivity is often caused by manic episodes which
allow the individual to have higher energy and need less sleep. This
often increases the likelihood of burnout. Confidence in oneself
during manic episodes increases which allows them to believe that they have the
ability to achieve goals that are often unattainable. As their self
confidence grows, their energy increases, and they become more outgoing and
charming. This allows them to be the center of attention, “the life of
the party”. Euphoria describes the feeling of joy and excitement about
life. When they’re in a manic state, the awareness and experience of life
is enhanced to such a level that it is exaggerated. These feelings also
creates a perception of increased intellect and insight Although
there are many disadvantages associated with the illness, some patients risk
the negative effects by discontinuing treatment because they miss the positive
aspects involved with the disorder. This article illustrated the reasons why some
people choose to deny medical intervention.
Bipolar
disorder has held a negative connotation for many people. The social
stigma associated with this mental illness can be attributed to the fact that
the general public does not understand the illness. They are uninformed about
definition of bipolar disorder and make assumptions that do not necessarily
correlate with the facts. The illness has been linked to words such
as crazy, maniac, and madness causing negative reactions and fear. This
research paper emphasized the following categories: statistics,
diagnostic criteria, non-adherence to treatment, coping skills, and positive
attributes of the disorder. Although bipolar disorder is a
misunderstood disease with many negative and positive aspects, it can be
managed with knowledge, understanding, and patience.
Works Cited
“Bipolar Disorder.” Umm.edu. University of Maryland Medical Center. n.d. Web. 18 Jan.
2014.
“Bipolar Disorder Statistics.”
Dbsalliance.org. Depression and Bipolar Support Alliance. n.d. Web. 18 Jan. 2014.
“Bipolar Disorder Statistics.” Statisticbrain.com.
Statistic Brain. Jul. 2012. Web. 18 Jan.
2014.
Duckworth, Ken. “Understanding Bipolar
Disorder and Recovery.” Nami.org. National
Alliance of Mental Illness, Aug. 2008. Web.
23 Jan. 2014.
Gibson, Susanne, et al. “Understanding
Treatment Non-adherence in Schizophrenia and
Bipolar Disorder: A Survey of What Service Users Do and
Why.” BMC Psychiatry 13.1 (2013): 1-12. Academic
Search Premier. Web. 18 Jan. 2014.
Goodwin, Guy M., et al. “ECNP Consensus
Meeting. Bipolar Depression. Nice, March
2007.” European Neuropsychopharmacology 18 (2008):
535-549. Academic Search Premier.
Web. 11 Jan. 2014.
Hong, Jihyung, et al. “The Cost of Relapse for
Patients with a Manic/Mixed Episode of
Bipolar Disorder in the EMBLEM Study.” Pharmacoecomonics
28.7 (2010): 555-566. Academic Search
Premier. Web. 14 Jan. 2014.
Jamison, Kay R. Touched with Fire. New York: Simon & Schuster, 1993. Print.
Látalová, Klára. “Insight in Bipolar
Disorder.” Psychiatry Quarterly 83 (2012): 293-310.
Academic Search Premier.
Web. 18 Jan. 2014.
Lowe, Chelsea and Bruce M. Cohen. Living with Someone Who’s Living with
Bipolar
Disorder: A Practical Guide for Family,
Friends, and Coworkers. San Francisco:
Jossey-Bass. 2010. Print.
Peay, Holly L., et al. “Adaptation to Bipolar
Disorder and Perceived Risk to Children: A
Survey of Parents With Bipolar Disorder.” BMC Psychiatry
13.1 (2013): 1-18. Academic Search
Premier. Web. 18 Jan. 2014.
Pedersen,
Tracy. “Benefits of Bipolar Disorder?” Psychcentral.com. Psych Central. May
2012. Web. Jan. 23, 2014.
Vann, Madeline. “Is There a Bright Side to
Bipolar Disorder?” Everydayhealth.com.
Everyday Health Media, LLC. n.d. Web. 23 Jan.
2014.
Images Cited
becauseilive. “How to Tell if You Have Bipolar Disorder.” Hubpages.com. Hubpages,
Apr. 2012. Web. 23 Jan. 2014.
“Causes
of Depression (Sociological, Physical, Psychological Causes).”
Trialx.com.
Cure Talk. Jul.
2013. Web. 21 Jun. 2014.
Khalife, Sami, Vivek Singh, and David J. Munzina. “Bipolar Disorder.”
Clevelandclinicmeded.com. The Cleveland Clinic Foundation. Aug. 2010. Web. 23 Jan. 2014.